Fracture Type Checker
Find Your Fracture Type
This tool helps identify common orthopedic fracture types based on injury mechanism and location. Click "Identify Fracture" to see your results.
Key Takeaways
- Fractures account for the highest share of orthopedic emergencies worldwide.
- The distal radius (wrist) fracture tops the list in most emergency departments.
- Prompt diagnosis with X‑ray, proper immobilisation, and early specialist referral are crucial.
- Open or displaced fractures often need surgical fixation, while many closed fractures heal with a cast.
- Understanding the typical patterns helps patients and clinicians act quickly and avoid complications.
Walking into an emergency department (ED), you’ll hear the rush of urgent cases. Among the buzz, one question often pops up: what is the most common orthopedic emergency? The answer guides how hospitals stock supplies, how doctors prioritize, and how patients prepare for recovery. In this article we break down the data, explain why certain injuries dominate, and walk you through the whole chain-from the moment the injury happens to the follow‑up care after the cast comes off.
Defining an Orthopedic Emergency
An Orthopedic emergency is a sudden musculoskeletal injury that threatens limb viability, neurovascular integrity, or long‑term function if not treated promptly. Typical triggers include high‑energy trauma (car crashes, falls from height), sports collisions, and severe twists. The core goal is to stabilise the anatomy, relieve pain, and prevent permanent damage.
Why Fractures Dominate the Emergency Landscape
When you look at ED logs across continents, fractures consistently surface as the leading cause of orthopedic presentations. A 2023 multi‑center study covering 12 hospitals in the United States reported that fractures represented 42 % of all musculoskeletal emergencies, followed by dislocations (13 %) and soft‑tissue injuries (9 %). In India, a recent survey from the All India Institute of Medical Sciences (AIIMS) showed 38 % of orthopedic admissions were fracture‑related, with the majority arriving via ambulance within two hours of injury.
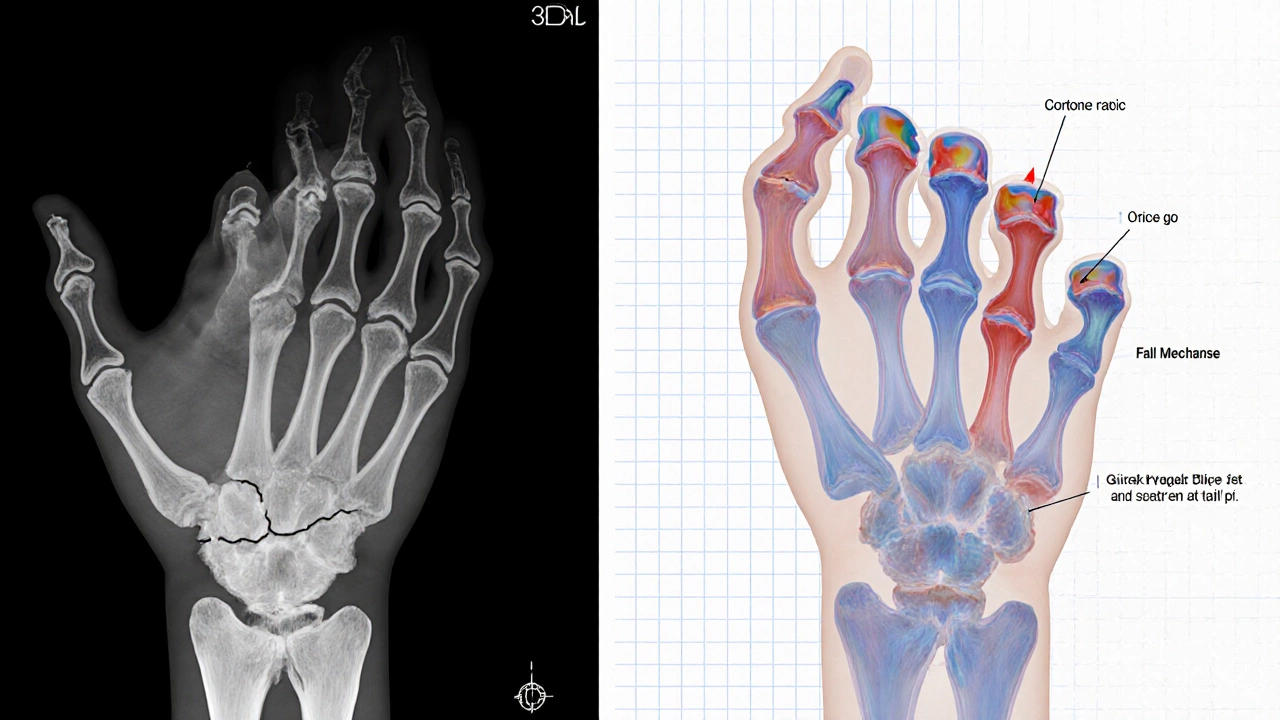
The Top Contender: Distal Radius (Wrist) Fracture
The Distal radius fracture tops the chart in most emergency departments, especially in adults over 55 and in children stretching out to break a fall. Its prevalence stems from two factors:
- Fall frequency: Worldwide, falls are the leading cause of non‑fatal injuries. The wrist is the first point of contact for many forward falls.
- Bone geometry: The distal radius is relatively thin and experiences high bending forces, making it vulnerable to breaks even with modest impact.
In the UK National Health Service data (2022), distal radius fractures accounted for roughly 18 % of all ED orthopedic cases, translating to more than 250,000 visits annually.
Other Frequently Seen Orthopedic Emergencies
| Fracture | Typical Age Group | Key Mechanism | Urgency Level |
|---|---|---|---|
| Distal radius | Children & seniors | Fall onto outstretched hand | High |
| Hip (proximal femur) | Adults >70 | Low‑energy fall | High (risk of avascular necrosis) |
| Clavicle | Young adults | Direct blow or fall onto shoulder | Medium |
| Tibia shaft | Teenagers | Motorcycle or sports impact | High |
| Open fracture (any bone) | All ages | High‑energy trauma with skin breach | Critical (infection risk) |
How Fractures Are Diagnosed in the ER
Speed and accuracy are vital. The diagnostic pathway usually follows these steps:
- Clinical assessment: Look for deformity, swelling, bruising, and evaluate distal pulses and nerve function.
- Imaging: X‑ray remains the first‑line tool. For complex joints (e.g., intra‑articular fractures), a CT scan adds detail; MRI is reserved for occult fractures or soft‑tissue injuries.
- Classification: Orthopedic surgeons use systems like AO/OTA to grade fracture pattern, displacement, and stability.
Time is of the essence. The American College of Surgeons recommends that definitive imaging be completed within 30 minutes for high‑risk injuries (open or vascular‑compromised fractures).
Initial Management: From Pain Relief to Immobilisation
Once a fracture is confirmed, the ED team follows a protocol that balances rapid pain control with protection of the injured segment.
- Pain control: IV opioids, NSAIDs, or regional nerve blocks, depending on patient factors.
- Reduction (if needed): For displaced fractures, a closed reduction is attempted under sedation or anesthesia.
- Immobilisation: Casting, splinting, or bracing. A cast is the gold standard for many distal radius and clavicle fractures.
- Antibiotics: Administered for open fractures within one hour to curb infection.
- Referral: A Orthopedic surgeon is consulted for definitive care, especially for surgical candidates.

When Surgery Becomes the Right Choice
Not every fracture needs a scalpel. Indications for operative fixation include:
- Open fracture with bone exposure.
- Displaced intra‑articular fractures where joint congruity is lost.
- Unstable fractures that cannot be maintained in a cast (e.g., comminuted distal radius).
- Fractures with associated neurovascular injury that require decompression.
Standard surgical options range from external fixation for severe open tibial fractures to internal fixation with plates, screws, or intramedullary nails for most long‑bone injuries.
Post‑ER Care: What Patients Should Expect
After the initial emergency visit, the recovery journey continues. Key points for patients include:
- Follow‑up appointments: Typically within 7‑10 days for cast check or wound inspection.
- Rehabilitation: Physical therapy starts once the fracture stabilises, focusing on range of motion and strengthening.
- Warning signs: Increasing pain, swelling, fever, or numbness may signal infection or compartment syndrome.
- Bone health: Calcium, vitamin D, and weight‑bearing exercises support healing, especially in older adults.
Quick Checklist for Emergency Staff
- Confirm neurovascular status before and after reduction.
- Obtain high‑quality X‑ray in at least two orthogonal planes.
- Apply appropriate analgesia; consider regional block for severe pain.
- Administer antibiotics within 60 minutes for open fractures.
- Document fracture classification and communicate clearly with orthopedics.
- Provide patient education on cast care and red‑flag symptoms.
What makes a fracture an orthopedic emergency?
Any break that threatens blood flow, nerve function, or the stability of a limb qualifies. Open fractures, displaced joint fractures, and fractures with accompanying compartment syndrome are high‑priority cases that need immediate attention.
Why is the distal radius fracture the most common?
The wrist is the first point of contact in many forward falls, especially among the elderly and children. Its thin bone structure and the force transmitted through the hand make it highly susceptible to breaking.
How quickly should an open fracture be treated?
Guidelines advise surgical debridement and antibiotic administration within the first hour of arrival to minimise infection risk.
Can all fractures heal without surgery?
Many simple, closed fractures heal well with casting or splinting. However, fractures that are displaced, involve joints, or are open often need operative fixation to restore alignment and function.
What are the red‑flag symptoms after a cast is applied?
Increasing pain, swelling, numbness, tingling, or a change in skin colour may indicate compartment syndrome or cast‑related circulation problems and require urgent evaluation.

 How Much Weight to Lose for Reversing Type 2 Diabetes?
How Much Weight to Lose for Reversing Type 2 Diabetes?
 Surviving Open Heart Surgery: How Rare Is Survival and What Are the Real Odds?
Surviving Open Heart Surgery: How Rare Is Survival and What Are the Real Odds?
 Success Rate of IVF: How Likely Is It to Work on the First Try?
Success Rate of IVF: How Likely Is It to Work on the First Try?
 Why Waking Up at 3 AM? Ayurveda Explains
Why Waking Up at 3 AM? Ayurveda Explains
 Hardest Type of Heart Surgery: What Really Tops the List?
Hardest Type of Heart Surgery: What Really Tops the List?