Cancer Treatment Matchmaker
How This Tool Works
Based on the information in this article, we've created a tool to help you understand which cancer treatments might be most appropriate for specific cancer types and characteristics. Select your cancer type, stage, and any available genetic information to see which treatments would be most commonly recommended.
Every year, millions of new cancer diagnoses hit headlines, but few people understand what actually makes a cancer cell keep dividing when it should quit. The good news? Our bodies and modern medicine have several ways to put the brakes on that runaway growth.
Quick Takeaways
- Cancer cells ignore normal cell‑cycle checkpoints and avoid programmed death.
- Tumor‑suppressor genes like p53 are the body’s natural "stop" button.
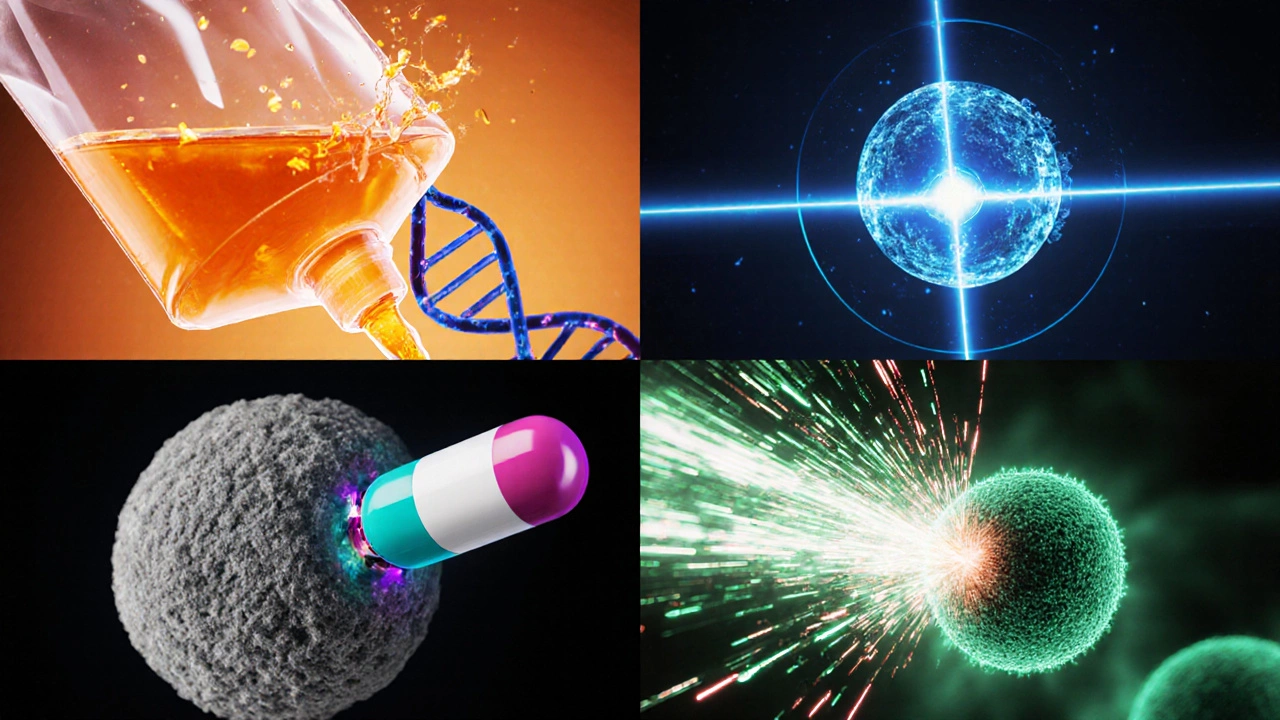
- Therapies such as Chemotherapy, radiation, targeted drugs, and immunotherapy each attack cancer growth in a distinct way.
- Blocking blood‑vessel formation (angiogenesis) and releasing the immune system from its brakes are newer, highly effective strategies.
- Lifestyle tweaks-quit smoking, maintain a balanced diet, stay active-support the body’s own defenses.
Why Cancer Cells Keep Growing
Cancer cells are cells that have accumulated genetic mutations allowing them to bypass the normal cell‑cycle checkpoints. They ignore signals that tell a healthy cell to stop dividing, repair DNA, or self‑destruct through apoptosis. This unchecked proliferation is the hallmark of a tumor.
Three core defects drive this behavior:
- Loss of tumor‑suppressor function.
- Constant activation of growth‑promoting pathways.
- Failure of programmed cell death (apoptosis).
Natural Body Defenses That Can Halt Tumors
Our DNA carries built‑in safety nets. Tumor suppressor genes encode proteins that monitor DNA integrity, pause the cell cycle, and trigger apoptosis when damage is too severe. The most famous of these is p53, often dubbed the “guardian of the genome.” When p53 senses DNA breaks, it can:
- Activate cell‑cycle checkpoints to give the cell time to repair.
- Induce Apoptosis if the damage is irreparable.
If tumor‑suppressor genes are mutated - a common event in many cancers - the “stop” signal is lost, letting the tumor grow unchecked.
Medical Interventions That Stop Cancer Growth
Modern cancer treatment leverages four main strategies, each working at a different point in the cancer‑growth pathway.
Chemotherapy
Chemotherapy uses cytotoxic drugs that damage DNA or interfere with cell division, affecting rapidly dividing cells the most. While effective, it also hits healthy rapidly dividing cells (like hair follicles), leading to side effects.
Radiation Therapy
Radiation therapy delivers high‑energy particles or waves (X‑rays, proton beams) that break DNA strands in tumor cells, triggering apoptosis. Precise targeting (e.g., IMRT) spares surrounding tissue.
Targeted Therapy
These drugs lock onto specific molecular abnormalities-such as HER2 over‑expression in breast cancer or BRAF V600E mutation in melanoma-blocking the pathways that tell the cell to multiply. Because they’re selective, side effects are generally milder than chemotherapy.
Immunotherapy
Immunotherapy awakens the body’s own immune system. Two popular classes are:
- Checkpoint inhibitors (e.g., PD‑1/PD‑L1 blockers) that lift the “brakes” on T‑cells, letting them recognize and kill cancer cells.
- CAR‑T cell therapy, where a patient’s T‑cells are engineered to target a tumor‑specific antigen.
Angiogenesis Inhibitors
Solid tumors need blood vessels to deliver oxygen and nutrients. Drugs like bevacizumab block VEGF signaling, starving the tumor and slowing its growth.
How the Options Stack Up
| Strategy | Primary Mechanism | Typical Use Cases | Common Side Effects |
|---|---|---|---|
| Chemotherapy | DNA damage & mitotic inhibition | Broad‑spectrum, solid & hematologic cancers | Hair loss, nausea, bone‑marrow suppression |
| Radiation Therapy | Localized DNA breaks | Localized tumors, brain, prostate | Skin irritation, fatigue, localized fibrosis |
| Targeted Therapy | Inhibits specific oncogenic proteins | HER2+, EGFR‑mutated NSCLC, BRAF‑mutated melanoma | Rash, diarrhea, liver enzyme elevation |
| Immunotherapy (Checkpoint Inhibitors) | Blocks PD‑1/PD‑L1 or CTLA‑4 pathways | Melanoma, lung cancer, renal cell carcinoma | Immune‑related colitis, pneumonitis, dermatitis |
| Angiogenesis Inhibitors | Blocks VEGF signaling | Colorectal, lung, renal cancers | Hypertension, bleeding, wound‑healing delays |
Lifestyle Factors That Support Medical Therapy
Even the most advanced therapies work best when the body’s baseline health is solid. Evidence shows that:
- Quitting smoking reduces the risk of treatment‑related complications by up to 30%.
- A Mediterranean‑style diet (rich in fruits, vegetables, whole grains, and omega‑3 fatty acids) can improve response rates in certain cancers.
- Regular moderate exercise (150min/week) boosts immune surveillance and may lower recurrence risk.

Common Myths and Pitfalls
Beware of “detox” teas or unproven supplements that claim to “starve” cancer cells. Most lack clinical data and can interfere with chemotherapy metabolism. Always discuss supplements with your oncologist.
Another trap: assuming a single treatment will eradicate every tumor. Cancer is heterogeneous; combination regimens (chemo+immunotherapy, for example) are often needed to cover multiple growth pathways.
Next Steps & Troubleshooting
If a chosen cancer treatment isn’t shrinking the tumor after a few cycles, doctors typically:
- Re‑biopsy to check for new mutations.
- Switch to a different targeted agent that hits the new mutation.
- Add a checkpoint inhibitor to rekindle the immune response.
- Consider clinical trial enrollment for cutting‑edge therapies.
Open communication with your care team, regular imaging, and blood‑marker monitoring are essential to catch resistance early.
Frequently Asked Questions
Can diet alone stop cancer cells from growing?
Diet alone can’t eradicate cancer, but a healthy eating pattern supports the immune system and may improve how well treatments work. It’s a complementary, not a replacement, strategy.
What’s the difference between chemotherapy and targeted therapy?
Chemotherapy attacks any fast‑dividing cell, healthy or cancerous, leading to broader side effects. Targeted therapy homes in on a specific molecular abnormality found only in the tumor, sparing most normal cells.
Why do some patients respond better to immunotherapy?
Response often depends on how many mutations the tumor has (higher “neo‑antigen” load makes it more visible to T‑cells) and whether the tumor expresses PD‑L1. Those factors help doctors predict benefit.
Are there risks to blocking blood‑vessel growth?
Yes. Anti‑angiogenic drugs can cause high blood pressure, bleeding, and slower wound healing. Doctors monitor these effects closely and may adjust doses.
What should I do if my tumor grows despite treatment?
Talk to your oncologist about re‑staging scans, genetic re‑testing, and possibly switching to a different regimen or enrolling in a clinical trial. Early detection of resistance is key.

 Complimentary Health Check-Up: Meaning, Inclusions, Benefits, and How to Use It (India 2025)
Complimentary Health Check-Up: Meaning, Inclusions, Benefits, and How to Use It (India 2025)
 Fastest Recovery Tips After Knee Replacement: Proven Strategies That Work
Fastest Recovery Tips After Knee Replacement: Proven Strategies That Work
 Heart Surgery Life Expectancy: What to Expect After the Procedure
Heart Surgery Life Expectancy: What to Expect After the Procedure
 Foods That Should Not Be Eaten Together According to Ayurveda
Foods That Should Not Be Eaten Together According to Ayurveda
 Are Ayurvedic Medicines Safe? Truths, Myths, and What You Need to Know
Are Ayurvedic Medicines Safe? Truths, Myths, and What You Need to Know