Knee Replacement Recovery Timeline Calculator
Recovery Progress Tracker
Your Recovery Timeline
Current Stage: Week 1
You're in the immediate aftermath phase. Pain is typically managed with IV or oral medications.
10% of recovery completed
Next Stage: Week 2-3
Pain decreases significantly but swelling peaks around day 5. You may still need over-the-counter pain relief.
25% of recovery completed
Key Milestones
Important Insight
By 6 months, 85% of patients report manageable pain. This is normal - your knee isn't healing at a linear pace. Recovery isn't about pain disappearing but about learning to manage it while rebuilding strength.
Recovery Factors
These factors affect how quickly pain subsides:
- Activity Level: Walking daily significantly speeds recovery
- Weight: Every extra pound adds 3-4 pounds of pressure
- Smoking: Reduces blood flow; smokers take 30% longer to recover
- Expectations: Unrealistic expectations cause unnecessary stress
After a total knee replacement, most people expect the pain to vanish quickly. But the truth? It doesn’t work that way. The sharp, stabbing pain from arthritis might be gone right after surgery, but the deeper, dull ache, swelling, and stiffness? Those stick around longer than many expect. So how long until your knee stops hurting? The answer isn’t a single number-it’s a journey, and everyone walks it at their own pace.
First 2 Weeks: The Immediate Aftermath
- Day 1 to 3: Pain is managed with IV or oral medications. You’ll feel sore, not sharp. The surgical site feels tight, like a deep bruise.
- Day 4 to 7: Most patients stop strong painkillers and switch to over-the-counter options like acetaminophen or ibuprofen. Walking with a walker or crutches becomes easier, but each step still triggers discomfort.
- Week 2: Swelling peaks around day 5 and starts to drop. You might notice the knee feels warmer than the other one. This isn’t infection-it’s normal inflammation. Pain at this stage is usually a 3 to 5 out of 10, mostly during movement.
Doctors often say, “If you’re not in pain at rest by week two, you’re doing well.” That’s a good benchmark. But don’t be surprised if you still need pain relief after walking to the bathroom or doing your first physical therapy session.
Weeks 3 to 6: The Transition Zone
This is where patience gets tested. The bone and soft tissues are healing, but your muscles are still weak. You might think you’re getting better, then hit a wall.
By week 4, many people stop using assistive devices. But here’s what’s not talked about enough: your knee still hurts when you sit for too long, stand up from a chair, or climb stairs. It’s not the old arthritis pain-it’s different. It’s the pain of rebuilding. Your quadriceps haven’t fired properly in months or years. Relearning how to use them takes time.
Studies tracking over 1,200 patients showed that 78% still reported mild to moderate pain at week 6. That’s not failure. That’s normal. The pain isn’t getting worse-it’s just not gone yet. Physical therapy is critical now. Skipping sessions because “it still hurts” is the biggest mistake people make.
Months 2 to 6: The Real Recovery Window
By month 3, most patients can walk without a limp and drive again. But the knee still feels stiff in the morning. It aches after a long day of standing. Climbing stairs still takes effort. This is the phase where people start asking, “Will this ever feel normal?”
Here’s what the data says: 60% of patients report significant pain reduction by month 3. By month 6, that number jumps to 85%. The pain isn’t gone-but it’s manageable. It’s no longer the kind that keeps you up at night. It’s the kind you notice when you’re walking the dog or doing yard work.
One patient in Bangalore, a 68-year-old retired teacher, told her physiotherapist: “It doesn’t hurt like before, but it’s not my old knee.” That’s the goal. You’re not getting back your 25-year-old knee. You’re getting a new one that works.
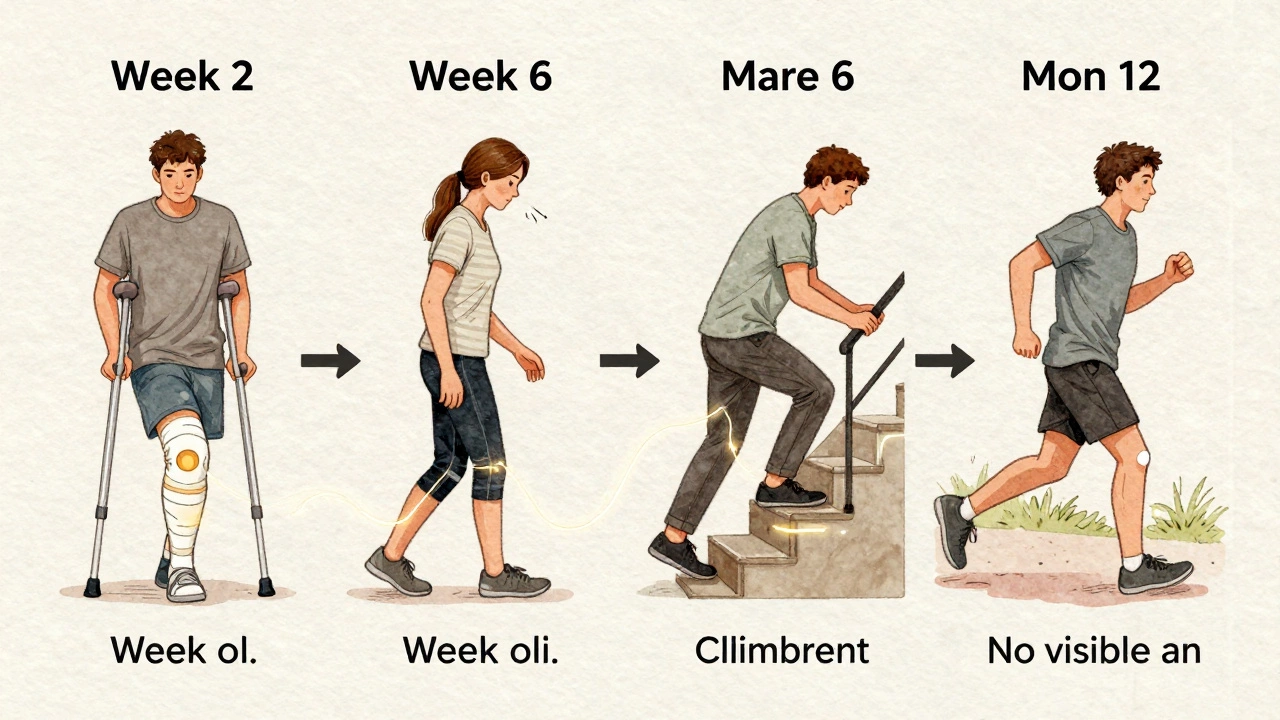
Months 6 to 12: The Final Stretch
This is when most people finally feel like themselves again. By 9 months, 92% of patients report minimal to no pain during daily activities. The remaining 8% usually have other issues-like arthritis in the other knee, obesity, or nerve sensitivity.
At 12 months, your knee should feel stable. You can walk for 30 minutes without stopping. You can kneel down (if you need to) without sharp pain. The swelling is gone. The stiffness is gone. The ache? It’s rare, and only after unusual activity.
Some people say their knee feels better than before. Others say it’s just “different.” Both are true. The artificial joint doesn’t have nerves like your natural one. So you won’t feel the same subtle sensations. But you won’t feel the grinding, burning pain of bone-on-bone arthritis either.
Why Does It Take So Long?
It’s not just the bone. It’s the ligaments, tendons, muscles, and even the nerves around the knee. During surgery, the surgeon cuts through soft tissue to get to the joint. That tissue needs to heal. And healing isn’t linear. There are good days and bad days. Rainy days make it worse. Cold weather stiffens it. Stress makes pain feel worse.
Also, nerve sensitivity can linger. Sometimes, the nerves around the knee get irritated during surgery. That can cause tingling, burning, or odd sensations for months. It’s not damage-it’s just the nerves recalibrating. Most cases resolve by 9 months.
What Delays Recovery?
Not everyone heals at the same speed. Here are the top five things that slow down pain relief:
- Being inactive: Skipping physical therapy or walking too little. Muscles atrophy fast after surgery.
- Being overweight: Every extra pound adds pressure to the new joint. Losing even 5% of body weight cuts pain significantly.
- Smoking: Nicotine reduces blood flow to healing tissues. Smokers take 30% longer to recover.
- Pre-existing nerve pain: If you had sciatica or diabetic neuropathy before surgery, you’re more likely to feel lingering discomfort.
- Unrealistic expectations: Thinking the knee should feel perfect by week 4 leads to frustration-and sometimes unnecessary doctor visits.

When Should You Worry?
Some pain is normal. Some isn’t. Call your surgeon if:
- Pain suddenly gets worse after week 6.
- You have redness, warmth, or drainage from the incision.
- You have a fever above 100.4°F (38°C).
- Your leg swells suddenly, especially in the calf.
- Pain wakes you up at night and doesn’t improve with medication.
These could be signs of infection, blood clots, or implant issues. Don’t wait. Get checked.
What Can You Do to Speed Things Up?
There’s no magic trick, but these habits make a real difference:
- Walk daily-even 10 minutes helps.
- Do your prescribed exercises, even on days you don’t feel like it.
- Ice your knee for 15 minutes after activity, especially in the first 3 months.
- Elevate your leg when sitting to reduce swelling.
- Stay hydrated and eat protein-rich foods. Healing needs fuel.
- Get enough sleep. Your body repairs itself while you rest.
One patient I spoke with started doing seated leg lifts every morning before coffee. After 6 weeks, she said, “I didn’t notice it until one day-I could stand up from the floor without using my hands.” That’s the kind of progress that sneaks up on you.
Final Reality Check
Most people expect their knee to feel normal by 3 months. The reality? It takes 6 to 12 months for the pain to truly fade. And even then, you might feel a slight ache after a long walk or a cold day. That’s not a problem-it’s just the new normal.
Your knee replacement isn’t a cure-all. It’s a tool. It removes the bone damage. But you still have to rebuild the strength, flexibility, and confidence around it. That takes time. And patience.
So if you’re 4 months in and still hurting? You’re not behind. You’re right on track.
Is it normal to have pain 6 months after knee replacement?
Yes, it’s normal. By 6 months, most patients have minimal pain during daily activities, but mild discomfort after extended walking, climbing stairs, or in cold weather is common. The pain is usually dull and fades with rest. If it’s sharp, sudden, or worsening, see your doctor.
Why does my knee hurt more at night?
At night, there are fewer distractions, so you notice the ache more. Also, inflammation builds up during the day from activity, and lying flat can cause fluid to pool around the knee. Ice before bed, elevate your leg, and take your evening pain medication as prescribed.
Can I run after a total knee replacement?
Most surgeons advise against running. The impact can wear down the artificial joint faster. Walking, swimming, cycling, and elliptical training are better options. If you’re determined to run, discuss it with your surgeon first-some patients with low body weight and strong muscles can do it cautiously after 12 months.
Does weight affect how long pain lasts?
Absolutely. Every extra pound adds 3 to 4 pounds of pressure on your knee with each step. Patients who lose 10% of their body weight before surgery recover faster and report less pain long-term. Even losing 5 pounds after surgery makes a noticeable difference.
Will I ever feel like I did before arthritis?
You won’t feel exactly like you did before arthritis, but you’ll feel better than you have in years. The goal isn’t to return to your 20s-it’s to return to a life without constant pain. Most patients say they can now do things they gave up-playing with grandchildren, gardening, walking to the market. That’s the win.

 What to Eat First in the Morning According to Ayurveda
What to Eat First in the Morning According to Ayurveda
 Pitta Person Traits: What Sets Them Apart in Ayurveda
Pitta Person Traits: What Sets Them Apart in Ayurveda
 What Is the Fastest Killing Cancer?
What Is the Fastest Killing Cancer?
 Can Christians Take Herbs? A Practical Guide to Herbal Supplements and Faith
Can Christians Take Herbs? A Practical Guide to Herbal Supplements and Faith
 Understanding Knee Pain: When is Knee Replacement Necessary?
Understanding Knee Pain: When is Knee Replacement Necessary?