When you hear about knee replacement surgery - also called total knee arthroplasty - you probably picture a quick fix that lets you run again. It’s a surgical procedure that replaces damaged knee joint surfaces with artificial implants.
Why the hype can be misleading
Marketing sheets often claim a "90% success rate" and a "back to normal life in six weeks". Those numbers look great until you dig into the fine print. Studies from the American Academy of Orthopaedic Surgeons (AAOS) show that about 15‑20% of patients need a revision surgery within 10‑15 years, especially if they’re younger or very active.
Implant lifespan - it’s not forever
Most implants are built from cobalt‑chrome alloys, titanium, or highly cross‑linked polyethylene. While manufacturers tout a 20‑year lifespan, real‑world data indicates that the average survivorship drops to 85% after 15 years for patients under 65. Implant materials matter: ceramic components have lower wear rates but are costlier and can be more brittle.
Hidden health risks you won’t hear in the brochure
- Blood clot formation: Deep‑vein thrombosis (DVT) occurs in 1‑2% of cases despite prophylactic anticoagulation. The risk spikes if you’re overweight, smoke, or have a prior clot history.
- Post‑operative swelling: Persistent edema can linger for months, affecting gait and increasing fall risk.
- Infection: Even with sterile technique, infection rates hover around 1% for primary procedures and climb to 5% for revisions.
- Stiffness and limited range of motion: About 10% of patients report that they never regain full flexion.
Recovery timelines are often optimistic
Doctors may say you’ll be walking unaided in a week, but functional recovery usually follows a "bone healing curve" that peaks around 12‑16 weeks. Physical therapy is not optional - it’s a full‑time commitment for the first three months, often five days a week.
Cost surprises beyond the surgeon’s fee
Many patients focus on the quoted surgery price, overlooking ancillary expenses like:
- Pre‑operative imaging (MRI, CT) - $500‑$1500 each.
- Hospital stay - $2,000‑$5,000 for a typical three‑day admission.
- Post‑operative rehabilitation - $100‑$250 per session, totaling $4,000‑$8,000.
- Potential revision surgery - can double the original cost.
Insurance may cover the primary procedure but often caps rehab sessions, leaving you to shoulder the balance.

Robotic‑assisted surgery: hype vs. reality
Robotic platforms promise up to 1‑mm accuracy in bone cuts. While that sounds impressive, a 2023 meta‑analysis found no significant difference in long‑term functional scores compared to conventional techniques. The main benefit is reduced intra‑operative variability, which matters mainly for high‑volume surgeons.
Choosing the right surgeon - what really matters
Volume matters more than fame. Surgeons who perform >50 knee replacements a year have a 30% lower revision rate. Look for board certification, hospital affiliation with an accredited orthopedic center, and transparent outcomes data.
Patient‑selection criteria you should discuss
Not everyone is a perfect candidate. Ideal patients are:
- Age 60‑75 with moderate arthritis.
- Body mass index (BMI) below 35.
- Non‑smokers with controlled diabetes.
- Motivated for intensive rehab.
If you fall outside these ranges, ask the surgeon how they’ll mitigate increased risks.
Quick checklist before you sign the consent form
- Confirm implant type and material.
- Ask about surgeon’s annual knee‑replacement volume.
- Request a written rehab schedule and total cost estimate.
- Discuss blood‑clot prophylaxis plan.
- Understand the signs of infection and when to call the clinic.
Bottom line
While knee replacement can dramatically improve quality of life, the truth is that success depends on implant choice, surgeon experience, realistic rehab expectations, and awareness of hidden costs and risks. Armed with this knowledge, you can have an honest conversation with your doctor and make a decision that’s right for your body and budget.
Frequently Asked Questions
How long does a knee replacement implant usually last?
For patients over 65, implants often last 15‑20 years. Younger, very active individuals may see wear as early as 10‑12 years, increasing the chance of revision surgery.
What are the most common complications after knee replacement?
The top complications include infection (≈1%), blood clots (1‑2%), persistent pain, limited range of motion, and stiffness. Early mobilization and proper anticoagulation reduce many of these risks.
Is robotic‑assisted knee replacement worth the extra cost?
Current evidence shows no clear long‑term functional advantage over conventional surgery. The extra cost may be justified for surgeons seeking higher precision, but it’s not a guarantee of better outcomes.
How soon can I return to normal activities?
Light activities like short walks often begin within a week. Full return to moderate exercise typically takes 3‑4 months, while high‑impact sports may be discouraged indefinitely.
What factors increase the chance of needing a revision surgery?
Younger age at the time of primary surgery, high activity level, obesity, and certain implant designs (especially early‑generation models) raise revision risk.
Comparison: Cemented vs. Cementless Implants
| Feature | Cemented | Cementless |
|---|---|---|
| Fixation method | Bone cement creates immediate bond | Porous surface encourages bone ingrowth |
| Typical patient age | Older, lower activity | Younger, higher activity |
| Long‑term survivorship | ~90% at 15 years | ~95% at 15 years (if bone ingrowth succeeds) |
| Risk of early loosening | Low if cement applied correctly | Higher if bone quality poor |
| Revision complexity | More bone removal needed | Potentially easier if bone ingrown |
Next steps if you’re considering surgery
- Schedule a comprehensive pre‑op evaluation with an orthopedic specialist.
- Request detailed outcome statistics from the surgeon’s practice.
- Arrange a meeting with a physical therapist to outline a rehab plan.
- Verify insurance coverage for the procedure, implants, and post‑op therapy.
- Discuss pain‑management options, including multimodal analgesia and nerve blocks.

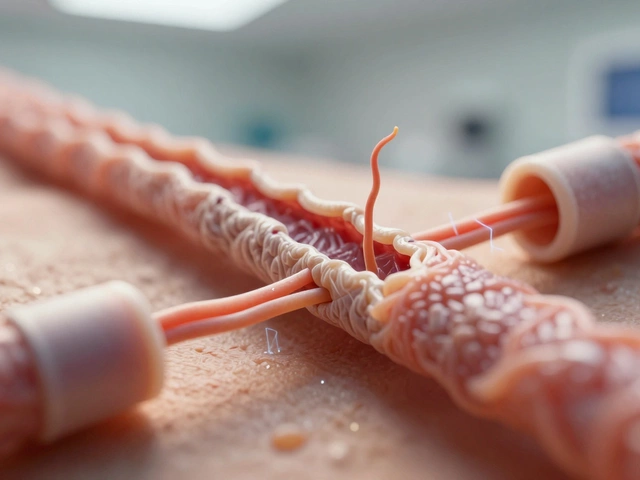 Can My Nerve Damage Be Repaired? What You Need to Know Now
Can My Nerve Damage Be Repaired? What You Need to Know Now
 Heart Surgery Life Expectancy: What to Expect After the Procedure
Heart Surgery Life Expectancy: What to Expect After the Procedure
 Complimentary Health Check-Up: Meaning, Inclusions, Benefits, and How to Use It (India 2025)
Complimentary Health Check-Up: Meaning, Inclusions, Benefits, and How to Use It (India 2025)
 How Do IVF Babies Look? Real Facts vs. Myths
How Do IVF Babies Look? Real Facts vs. Myths
 What Is the Best Herb to Take Daily? Top Choices Backed by Science
What Is the Best Herb to Take Daily? Top Choices Backed by Science